Varicose Vein Treatment – Understanding Your Options

Reviewed by Mitchel P. Goldman, MD
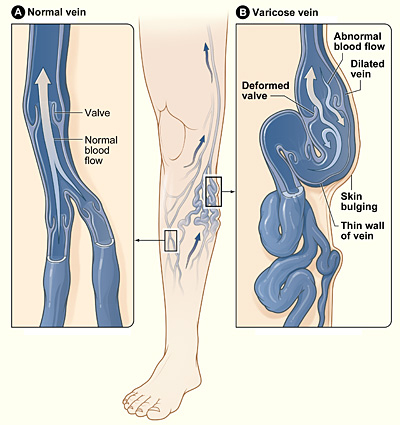
Varicose veins are swollen, raised and twisty; some can be very large and dark blue in color. These unsightly veins usually occur in the legs, but they can also develop on the hands, face and breasts. An estimated 30 million Americans aged 18 to 70 have varicose veins, 50 percent of whom experience blood clots, phlebitis (inflammation of the veins) or ulcerations. Varicose veins may also cause night cramps, restless legs, pain and ankle swelling.
Now that you understand the symptoms associated with varicose veins, it’s time to learn what actually causes them.
Varicose Vein Causes
All veins have one-way valves that help keep blood flowing toward the heart. When these valves become weak or damaged, blood backs up and pools in the veins, causing them to enlarge into varicose veins.
There are many potential causes of the damage that leads to varicose veins. This list includes family history, age, gender, pregnancy, excess weight, a sedentary lifestyle and leg trauma. If you are concerned about varicose veins, schedule a consultation with a doctor who has experience treating problem veins. He or she will perform a specialized ultrasound exam to map blood flow in the veins and identify where the blood is backing up and pooling (reflux). This exam can diagnose the condition and help your doctor choose the most appropriate treatment for you. Your doctor may suggest a trial period during which you wear compression stockings to see if the symptoms resolve, before moving on to more aggressive therapies.
By National Heart Lung and Blood Institute. (Varicous veins.)
[Public domain], via Wikimedia Commons
Varicose Vein Treatments
Previously, the only way to get rid of varicose veins was through invasive vein stripping and ligation surgery, through which the large vein in the leg (the great saphenous vein) is tied (ligation) and/or removed (stripping). These major surgeries are usually reserved for the most severe cases of varicose veins.
Vein stripping and ligation takes about 60 to 90 minutes to perform and sometimes requires general anesthesia. Recovery time is also lengthy, usually involving two to four weeks depending on how many veins were stripped and where they were located.
Vein stripping surgery costs between $1,500 and $3,000. This cost may not include additional fees charged by the hospital or surgical center, which can increase the cost exponentially.
Another varicose vein-removing surgery is called ambulatory phlebectomy. During this procedure, your doctor makes tiny cuts in the skin to remove small varicose veins; usually those that are closest to the surface. The in-office procedure is done with local anesthesia and is considered much less invasive than vein stripping and ligation.
Ambulatory phlebectomy may cost between $1,000 and $3,000 per leg depending on the extent and number of veins removed.
Endovenous Laser Ablation
Laser therapy for varicose veins taps into laser or high-frequency radio-wave energy to heat and close the problem vein. The veins are left in place so there is minimal bleeding and bruising. There is also no cutting involved. Laser vein surgery is less painful and involves significantly less downtime than ligation and stripping, with similar cosmetic results. These procedures are performed in the doctor’s office under local anesthesia. You can leave the office and walk immediately after the procedure.
On average, endovenous laser or radiofrequency ablation costs $3,000 to $5,000 based on how much of the vein needs to be treated and where the practice is located. Large cities like New York City and Miami may charge more, as overhead is generally higher in these urban areas.
Sclerotherapy
Sclerotherapy involves injecting a solution directly into the varicose vein, which irritates the lining of the blood vessel, causing its destruction. Gradually, the vessel turns into scar tissue and fades away. Not everyone with varicose veins is a candidate for sclerotherapy. Further, the treatment is not usually recommended for the great saphenous vein because it has a high recurrence rate and frequently requires multiple treatments.
Previously, sclerotherapy injections were always liquid based, but today they are also available as foam. Foam sclerotherapy involves mixing the same solution with air or carbon dioxide.
Varithena by BTG is a new foam sclerotherapy that was approved by the Food and Drug Administration in late 2013. The main advantage of foam sclerotherapy is that it displaces the blood in the vessel being treated. When this occurs, the solution directly contacts the vessel wall for a longer period of time than with a liquid solution. The enhanced solution-to-vessel wall contact allows the agent to work more effectively. The foam can also be seen via ultrasound, which helps guide and monitor the therapy.
The cost of sclerotherapy injections ranges from $500 to $650 depending on the extent of damage to the veins treated and the cost of the graduated compression stocking (around $100), which must be worn after treatment to maximize results.
Varithena foam injection costs range from $1,500 to $3,000 depending on the number of vessels treated.
The good news is that there are many effective treatments available to treat varicose veins today. Choose a qualified physician with experience treating varicose veins who can advise you on which is best based on your aesthetic or functional goals, budget and your ability to adhere to recovery instructions.
About the Reviewer of This Article
Mitchel P. Goldman, MD, is the founder and medical director of Goldman Butterwick Fitzpatrick Groff & Fabi: Cosmetic Laser Dermatology in San Diego. There, he directs the fellowship program accredited by the American Society for Dermatologic Surgery. He also is a Volunteer Clinical Professor in Medicine/Dermatology at the University of California, San Diego. Dr. Goldman is the 2013-14 President of the American Society for Dermatologic Surgery. He is founder and past president of the American College of Phlebology and past president of the San Diego Dermatological Society and the Sonoran Dermatology Society.
Spider Veins
Reviewed by Joshua L. Fox, MD
Spider veins (telangiectasias) are broken blood vessels or capillaries that appear on the skin’s surface as fine red lines. They affect about half of the women in the United States, and many men, too.
Spider Veins vs. Varicose Veins
Spider veins should not be confused with varicose veins. Unlike varicose veins, which are much larger, spider veins rarely cause substantial medical problems or complications, although they are unsightly and may burn, swell and ache. They appear near the surface of the skin on the legs or face. Spider veins get their name from their web-like appearance, although they can appear as single veins as well. They are considered primarily a cosmetic issue.
Varicose veins, on the other hand, are much larger and bulky in appearance. They’re filled with an abnormal collection of blood and are usually dark purple or blue in color, cord-like, twisted, bulging and often raised above the surface of the skin when they are symptomatic. Symptoms may include fullness, tingling, heaviness, aching, burning, throbbing and pain in the legs. Varicose veins also can lead to more serious medical conditions, including stasis dermatitis, bleeding (red, brown scaly rash on body), pitting edema (swelling from excess fluid), ulcers (from long-term fluid buildup in the tissues) and, rarely, blood clots (thrombophlebitis).
Spider Veins: Causes and Prevention
Spider veins are caused by several factors, including aging, weight gain, obesity, genetics, hormones (pregnancy and childbirth, birth control pills and estrogen replacement therapy), rosacea (a chronic skin condition that causes inflammation of the cheeks, nose, chin, forehead or eyelids), trauma to the leg, prolonged sitting or standing, and sun damage.
The best way to prevent spider veins is to avoid the triggers. For example, always wear sunscreen with a sun protection factor (SPF) of 15 or higher plus protection against the sun’s Ultraviolet A and Ultraviolet B (UVA and UVB) rays when outside. Maintaining a healthy weight, engaging in regular exercise and eating a high-fiber diet may also be protective. Wearing low-heeled shoes can help prevent spider veins in the lower extremities. Trying to shift your weight when you stand is helpful. The most effective nonsurgical treatment is support stockings, also known as compression stockings.
Spider Vein Treatment: Sclerotherapy
The current treatment for removing unwanted spider veins is an injection method known as sclerotherapy, which has been around since the 1930s. Sclerotherapy can be used to remove both unwanted spider veins and reticular veins (small varicose veins that are between 1 and 3 millimeters in diameter) in the ankles, calves and thighs. The goal of the treatment is to permanently remove the targeted veins and ease any symptoms they may be causing.
Best Candidates for Sclerotherapy
The best candidates for sclerotherapy are physically- and psychologically-healthy non-smokers who are well-informed about the treatment, have realistic expectations, and are fully able and motivated to comply with aftercare instructions.
People with certain medical conditions such as blood-borne, infectious and cardiac diseases, as well as those with high blood pressure or diabetes, may not be able to undergo sclerotherapy. Women who are pregnant are not candidates for sclerotherapy, but their spider veins may resolve naturally within months after childbirth.Nursing mothers are advised to postpone sclerotherapy treatment until their child is weaned.
Sclerotherapy: The Procedure
Sclerotherapy is performed on an outpatient basis at the doctor’s office or in an outpatient surgical setting. It does not require anesthesia, and discomfort is minimal. A sclerotherapy session lasts from 10 minutes up to an hour, depending on the number and size of veins being treated. Two or more sessions are usually needed to complete treatment with optimal results.
Prior to the procedure, the doctor will ask you to follow specific instructions such as refraining from using moisturizers, sunscreen or products containing oil in the area to be treated, or wearing shorts on the day of treatment. Following these preoperative instructions carefully will help the procedure go smoothly.
The doctor will discuss the type of solution (sclerosing agent, or sclerosant) that will be injected during the procedure. There are numerous solutions that can be used for sclerotherapy. One of the newest is Asclera (polidocanol), which received FDA approval in early 2010 for the treatment of spider veins and reticular veins in the lower extremities. Unlike other sclerosing agents, Asclera contains anesthetic, which may make the experience more comfortable. Your doctor will advise you on the appropriate solution for your condition.
During the sclerotherapy procedure, a bright light is directed at the vein as the doctor injects the sclerosing agent into it with a very thin needle. The sclerosant irritates the interior walls of the vein, which constrict, collapse and prevent the flow of blood. This simple action effectively eliminates any swelling, bulging, discoloration or discomfort that the spider and reticular veins may have caused. The vein fades within days to weeks.
Typically, each inch of vein requires an injection. A cotton ball is taped over each injection site; it can be removed after 48 hours. A compression stocking is often worn to support the treated areas once the procedure is over. Compression garments are a normal recovery aid for many procedures. It is extremely important that you wear this stocking as directed by your doctor to reduce the risk of bleeding, bruising, hyperpigmentation (discoloration) and blood clotting.
After the Sclerotherapy Procedure
Following your sclerotherapy treatment you may experience slight leg cramping within the first two days, but this discomfort is usually not strong enough to require medication. Itching can also occur and can be managed with medication.
The treated veins will look worse before they look better. There will be bruising that takes up to a month to clear up, so you may want to keep your legs under wraps until then. Your doctor may direct you to walk often for the first several days after the procedure to reduce the risk of blood clot formation. He or she may also instruct you to avoid sitting or standing for extended periods of time, and to limit your exercise routine for about a month.
Results will vary depending upon individual anatomy, how well you follow your doctor’s directions during the healing process, the specific sclerosing agent used, and the expertise of the doctor.
Complications and Risks
Complications from sclerotherapy are rare. The most common complication is a brownish-red discoloration in the treated area that usually resolves itself within a year. Matting of the veins can also occur, which shows up as red-colored blood vessels that require additional treatment to resolve. Other rare complications include deep vein thrombosis (blood clots), inflammation, ulceration, scarring, allergic reaction to the injected solution, and reappearance of spider veins.
Facial Spider Veins: Laser Them Away
There are other, different treatments for spider veins on the face. The gold standard is laser therapy, which uses light to destroy the tiny blood vessels and restore the skin’s natural appearance. It’s quick (10-15 minutes), safe and produces immediate results.
The laser targets only the broken blood vessels, not the surrounding skin, and the success rate is up to 70 percent with the first treatment. However, new spider veins can appear afterward, requiring additional rounds with the laser.
Spider veins that lie deeper under the skin may be treated with intense pulsed light (IPL). This newer technique is similar to laser therapy in that it uses light energy to destroy the vein without damaging surrounding tissue. IPL is also used to eradicate small vascular birthmarks.
As with all cosmetic procedures, laser or IPL treatment of spider veins is rarely covered by medical insurance. It’s always best to check with your insurance provider to determine the terms of your policy prior to treatment.
Consult a Qualified Doctor
Dermatologists, vascular medicine specialists and plastic surgeons may be best qualified to use sclerotherapy and lasers to remove spider veins. Choose a doctor who has extensive training and experience with your procedure of choice. A qualified doctor will help you select the most appropriate treatment for your condition, increase the odds of success, and reduce the risk of complications.
Spider Vein Therapy Costs
Sclerotherapy cost includes two fees: the physician’s fee and the facility fee. Costs vary depending on the doctor, your geographic region, the type and extent of your procedure and other factors. The fees can start at about $225 per syringe of sclerosant. Patients may require one or two syringes per session, and treatment may need to be repeated to produce the best results.
Laser therapy costs run about $250 per session and up, depending on the area of treatment.
Because spider vein treatment is considered cosmetic, medical insurance does not cover the cost. If the cost of sclerotherapy or laser therapy is difficult for you, ask your doctor about payment plans and medical finance options. For financing options and tips, continue reading about patient financing.
About the Reviewer of This Article
Joshua L. Fox, MD, earned his medical degree from the Mt. Sinai School of Medicine in New York. He completed an internship at Maimonides Hospital in Brooklyn, followed by a three-year dermatology residency at the New York University School of Medicine. A Fellow of the American Academy of Dermatology, Dr. Fox is the founder and director of Advanced Dermatology, P.C. of New York and New Jersey and the Center for Laser and Cosmetic Surgery. He is a spokesman for both the American Academy of Dermatology and the American Society for Dermatologic Surgery. For more information on Dr. Fox, visit http://www.advanceddermatologypc.com